The rollout of the Patient Protection and Affordable Care Act is changing the face of healthcare delivery and reimbursements.
Here three spine surgeons discuss healthcare reform, its impact on reimbursements and whether Medicare will start reimbursing for spine procedures in ambulatory surgery centers in the near future.
Question: How has healthcare reform impacted reimbursement at your surgery center?

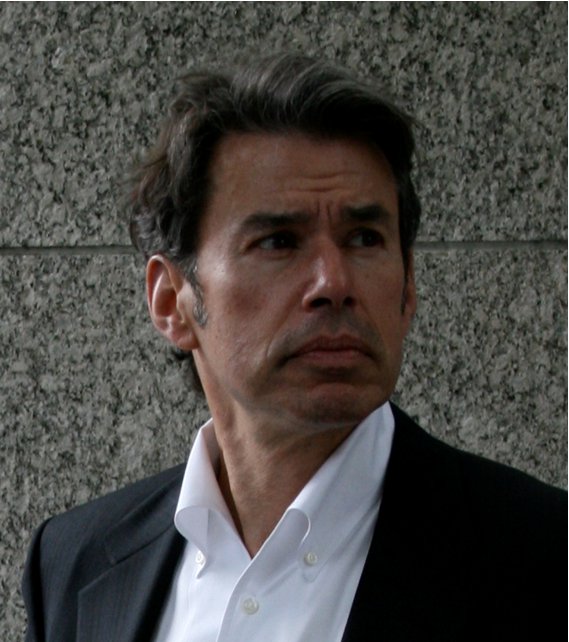
Fred F. Naraghi, MD, Comprehensive Spine Center, San Francisco: The new healthcare law has created a way to get insurance protection for a lot of people, which may be a good thing. But it has not changed the pricing structure. It's early to know what the full impact is. There is uncertainty as the premiums rise and the cost is shifted to tax payers.
The net effect at the surgery center has been lower volume and reduced reimbursements. We are also being more selective on some of the insurances. For example, although worker's comp may have a lower reimbursement, they tend to reimburse reliably. We're in a transitional phase as the new law is taking effect. So certain trends may develop in the next four to six months.
Richard Wohns, MD, Founder and President, NeoSpine, Seattle: Surgery center reimbursement seems to be totally untouched at this point, but what we think is that more cases will be driven towards the surgery center. This type of delivery of healthcare is what the industry wants and so it will not discourage this change by decreasing reimbursements. If the driving force is to get more cases into the surgery centers, then it is counter productive to reduce reimbursements thereby forcing centers to close.
Q: Are you seeing any change in which procedures insurance companies will approve for ASCs?
Dr. Naraghi: We have not seen any significant change in procedures yet. Certain procedures continue to be difficult to get insurance authorization for surgery centers, such as one-level ACDF. There is always a push to convince the carriers of the overall lower cost of doing the same procedure at the surgery center versus the hospital.
The one area that the new law needs to address, perhaps through an amendment, is to limit the current hospital monopoly and antitrust issues. Hospitals still can have enormous leverage with insurances and that increases the cost of healthcare.
Harvinder Bobby Bhatti, MD, Atlanta Orthopedic Institute: I think the number of procedures we are able to perform in the ASC is going to increase. Procedures such as single level cervical disc replacement, single level cervical fusions, laminectomies, will become outpatient. Also, more facilities will get observational units so that they can keep an eye on patients overnight. However, the problem may be increased volumes with lower reimbursement rates, which may cause many businesses to close.
Q: Is there anything you have changed to deal with reimbursement challenges?
Dr. Naraghi: We currently submit proactive appeal letters with our billing for the procedures to improve reimbursement. Also, we are being more selective in accepting some of the insurances. As an example, we have increased our worker's compensation patients to offset the lower reimbursements from the private insurers.
We are also monitoring reimbursement from CMS, to see if there would be need to consider discontinuing it.
Dr. Bhatti: I think a lot of us are thinking of ways to diversify our income. A lot of us are thinking of not taking the governmental health plans as we monitor the reimbursements; with the addition of other sources of income to offset the loss if we do accept the "under-insured."
Q: Do you think Medicare will start reimbursing for spine procedures in the ASC at any point?
Dr. Wohns: If they really looked into this they would. I just don't know if it is on their radar screen. They are really concerned about patient safety and they would have to be careful about who they approve for spine surgery.
There are a large number of Medicare beneficiaries who are healthy who need a simple procedure performed and who now have to go to the hospital and leave the same day, which costs three or four times more than if the procedure were done at an outpatient center. So if Medicare realizes that their beneficiaries are receiving outpatient procedures at hospitals but it's costing them so much more, maybe they will start reimbursing for ASC procedures as well.
Q: What are you preparing for in the coming year in terms of dealing with healthcare reform?
Dr. Naraghi: We are doing internal audits to make sure we remain compliant with HIPAA. We are continuing our "brand" marketing to remain busy in our highly competitive environment. We are reviewing and considering options in terms of discontinuing CMS, depending on reimbursements in the upcoming year.
Healthcare reform is going through its second phase currently. The first phase was the initial phase, from 2010 to 2013. The second phase is the market expansion, from 2014 to 2017. The third phase is the restructuring, from 2018 to 2020.
We anticipate a slow growth in spine services. We also anticipate deterioration in the payer mix, as the insurance premiums are increasing across the board. This may cause added constraints on private practices and a shift to hospital or group employment for orthopedic and neurosurgeons.
As the insurance coverage is expanding as of January 2014, about half of the 30 million Americans who are uninsured will be covered under Medicaid, which would cause a strain on the primary care physicians and emergency rooms. The impact is probably less intense on spine providers. The current law needs to be amended to control the exponentially increasing cost rather than simply shifting the cost to tax payers.
Specific areas that have not been addressed by the new law include: improving physician malpractice coverage issues, increasing the antitrust laws to prevent hospital domination of the markets and increasing taxes on their profits and controlling the pharmaceutical prices.
Dr. Bhatti: For us it's pretty simple. We are just looking to see what the reimbursements are going to be. The payments need to keep up with the cost of running a practice from the rising costs of malpractice insurance to the labor force to basic office overheads. We are a society of instant gratification, and if our delivery of spine care becomes two-tiered as in many countries, such as the United Kingdom, we will see a shift rise in many surgeons adopting different payment strategies. This may not immediately affect the already super-specialized spine community. I will not be surprised if at some point in the near future we have a system of those that can afford immediate care and those that can only afford care when it is financially feasible or regulated under the Affordable Care Act. The bottom line however is that we do not know what will happen as not many people I know have read the 10,535 pages of regulations published thus far.
More Articles on Spine Surgeons:
Dr. William Couldwell: 5 Considerations for Neurosurgeons in ACOs
Dr. Mark Kuper Joins North American Spine
Drs. Chad Prusmack, Stanley Herring Provide Spine Care for 2014 Super Bowl Teams

