Documentation is an important part of patient care and accurate documentation is essential for spine surgeons to receive payment on their procedures.
"It's important for surgeons to get a more accurate history and record of the patient during their first meeting," says Hamid Mir, MD, an orthopedic spine surgeon at DISC Sports & Spine in Marina Del Rey, Calif. "Then you can use the recorded information to make a clinical or surgical decision. If you have accurate documentation for patients, especially surgical patients, you can use that information for future treatment and right before surgery. If you accidentally record the wrong level or side in the documentation, then you'll increase the error rate."
Here are eight ways spine surgeons can improve their documentation.
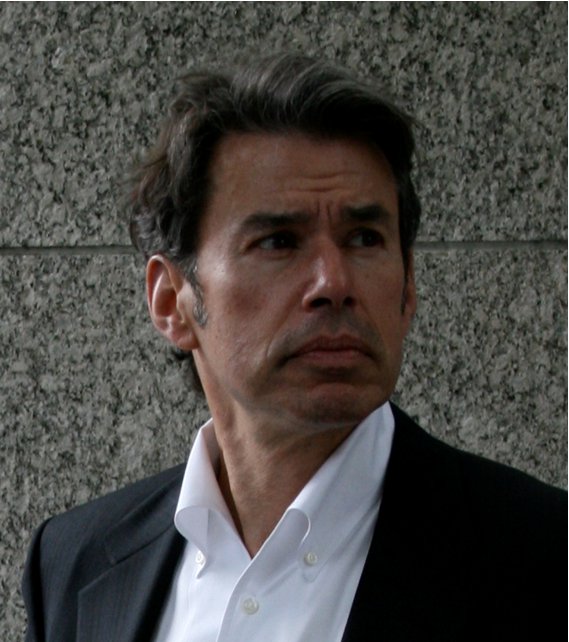
1. Task assistants to compile data. The surgeon has many responsibilities, so a nurse or another assistant should be tasked with gathering patient history and other data important for their records and documentation. "One of the assistants to the surgeon should gather data in advance of the patient visit and make sure it remains updated at all times," says Richard Wohns, MD, JD, MBA, founder of NeoSpine in the Puget Sound region of Washington. "The surgeon's responsibility is making sure the history is very specific and exam is thorough."
2. Detail patient histories. The EMR can help you track patient histories better than before. Make sure to dig into the details as deeply as possible. "A new history should be in incredible detail with all of their symptoms and what caused the pain," says Dr. Wohns. "If there was a cause such as a vehicular accident or work injury, include that as well. Indicate past surgical interventions and clearly delineate all imaging that has been done."
3. Include all imaging studies. If the patient has undergone prior imaging studies, acquire them before deciding on treatment. Otherwise, order new images or other diagnostic tests to pinpoint the issue and send the patient down the right treatment pathway. "The list of imaging studies patients have done is important," says Dr. Mir. "For spine surgeons, it's crucial to review the actual films themselves and not just rely on the radiologist reports."
These images are important for showing how the disease or treatment has progressed. "Have a record so you can see the evolution of the MRI or CT scans over time," says Dr. Wohns. "Also include longitudinal studies such as EMG studies in every record so you have the full history in repeated visits over time. This is evidence of neural dysfunction or improvement."
4. Take advantage of patient portals. Electronic medical records now often come with patient portals, which allow patients to enter their own electronic data. "This can improve the accuracy of the information and make sure it's timely," says Dr. Mir. "The patient fills out their history and every time they come in, they'll update with any changes to medications or other conditions. Additionally, if they are admitted to a hospital or experience another significant change with their health, we are notified. If an older patient is taking blood thinners they forgot to mention in their histories, it's nice to capture that electronically."
5. Use a pain diagram. Instead of just recording the patient's explanation of the pain, use a diagram for the patient to draw exactly where their pain is on the picture. "This is documentation from the patient that we like to use to review and make sure we have the right side and area of pain to cross-check my documentation," says Dr. Mir. "It helps with clinical decision-making. I also have my own set of questions about pain location, severity, associated complaints, weakness, sensory deficits and what treatments they've tried in the past."
6. Update assessments with subjective symptoms. Every exam should include a well thought out plan and assessment, recording subjective symptoms such as the patient's chief complaint. "Anything such as back pain and cervical radiculopathy or myelopathic symptoms have to be there," says Dr. Wohns. "Make the symptoms and radiological findings available so it's clear what the patient is complaining of and the summation of patient symptoms. Statements should be succinct and clear whether the treatment is surgical or not. Anyone reading the chart should know exactly what the surgeon is thinking."
7. Spell out plans in great detail. Treatment plans should be clear and concise in the patient's documentation and surgeons must ensure patients understand their plan before leaving the office. "Spell out in the medical record that the patient was advised to the plan and potential complications," says Dr. Wohns. "Record that patients understand their postoperative limitations and return-to-work schedule. This should all be spelled out by the surgeon in the clinical note. It's good for quality of care and could have medicolegal consequences. The plan should be spelled out on the record and verbally for the patient so there is know issue as to why the surgeon did what he did."
8. Make sure everyone involved in patient care gets updates. EMR has also made it easy to keep other specialists and primary care physicians informed about the patient's progress during treatment. "The EMR allows us to copy everyone else involved on the patient records, which are sent to them as soon as the patient is seen," says Dr. Mir. "The advances in EMR systems are really making information transfer more accurate and allowing us a safer way to practice medicine."
More Articles on Spine Surgery:
7 Access to Care Issues for Spine Patients & How Surgeons Can Overcome Them
10 Key Components of On-Call Contracts for Spine Surgeons
Introducing Continuity Into Spine Care: 5 Pillars of Salem Spine Center's Referral Program

