For more than 100 million Americans with chronic pain, finding an effective treatment can involve trying several different treatment options with each having very different clinical outcomes.1 At a recent roundtable discussion at the 2017 North American Neuromodulation Society Annual Meeting, leading experts in the field of pain management discussed how to improve the care continuum for patients with chronic pain and shared insights on recent research in spinal cord stimulation (SCS).
With long-term opioid prescriptions for chronic pain contributing to the nation’s opioid crisis, physicians are now evaluating how to treat chronic pain with options that reduce the over- reliance on opioids. One treatment option that many are revisiting is SCS which, since its introduction more than 40 years ago, has made great advancements in its ability to target pain and provide patients with long-term relief.
“When people think about pain management, it’s often synonymous with opioids,” said Julie Pilitsis, M.D., Ph.D., professor, neurosurgery and neuroscience and chair of the Department of Neuroscience and Experimental Therapeutics, Albany Medical College. “We have to expand our treatment options and medical treatments to include interactive therapies and SCS.”
In the discussion, which was moderated by Richard Rauck, M.D., founder, Carolinas Pain Institute, the panelists noted that there are a number of common conditions which indicates that a patient could be a candidate for SCS including failed back surgery syndrome and neuropathic pain. Patients with these conditions are frequently being treated with SCS.
“It’s critical to understand the root cause of a patient’s pain whenever possible. For a sizeable group of patients, SCS should be used earlier in the treatment algorithm, especially as the technology continues to advance to reach a broader range of patients with chronic pain,” said Dr. Rauck.
James North, M.D., pain specialist, Carolinas Pain Institute and assistant professor, Wake Forest University Baptist Medical Center added, “There is a vacuum of treatment options for neuropathic pain. Based on my clinical experience, SCS is an effective modality in treating the most refractory type of pain and that’s neuropathic pain.”
The evolution of spinal cord stimulation
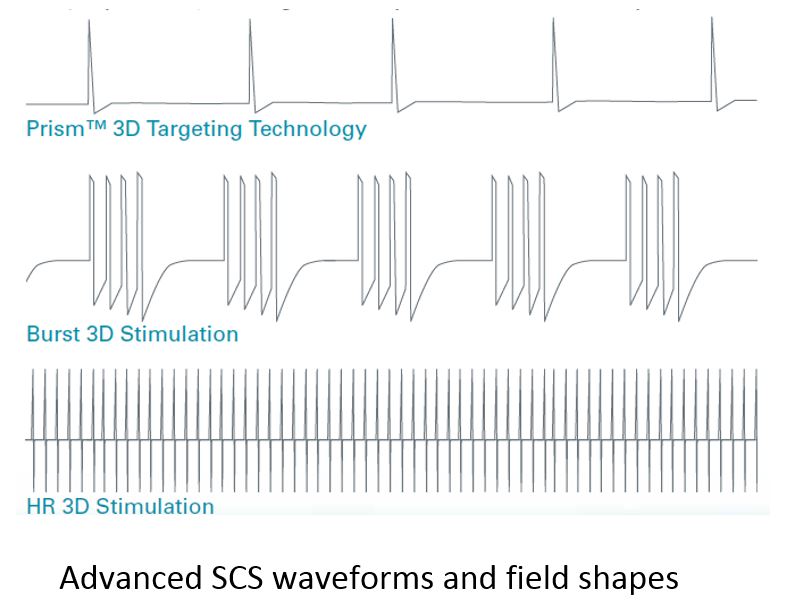
The most advanced SCS systems are designed to address many of the challenges of earlier models where patients would experience stimulation of adjacent non-targeted nerves or possibly become non-responsive to the treatment over time. Recent technology uses 3D neural targeting which is engineered to enable physicians to precisely target the area in the dorsal column that is intended to best treat the patient’s pain. Additionally, these systems can more readily respond to pain as it changes over time by delivering waveforms of different shapes, intensity, frequency and duration.
“What I’ve noted in my practice with spinal cord stimulation is the technique and the quality of the technology has advanced to the point that we’re having unprecedented success. It’s not uncommon for us to see 100 percent pain relief using this modality,” shared Stephen Pyles, M.D., founder, Pain Treatment Centers.
The Boston Scientific portfolio of SCS Systems with the Illumina 3D™ Programming Algorithm incorporates these latest innovations. Its technology is based on a 3D anatomical model of the spinal cord that takes into account the electrical conductivity of spinal column structures, relative
lead location and vertebral level of the leads. Using these inputs, the algorithm is intended to calculate the optimal fractionalized program configuration to target the selected central point of stimulation. Once the recommended neural target is identified, MultiWave™ Technology allows pain therapy to be further customized for each individual patient through the delivery of a variety of waveforms and field shapes.
In a recent device registry evaluation of data using the Boston Scientific Precision Spectra™ System, 60 percent of patients used one or more advanced waveforms to treat their pain.
"Given the complex nature of chronic pain, it stands to reason that one type of stimulation is unlikely to be the answer to all pain phenotypes," said Dr. Julie Pilitsis.
Research highlights
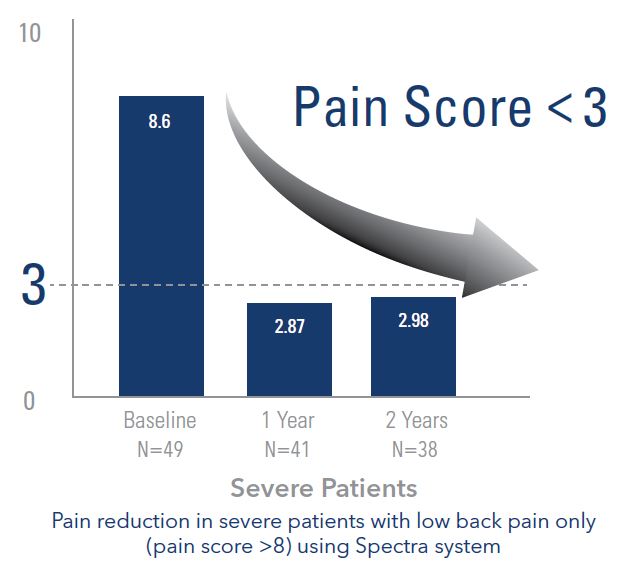
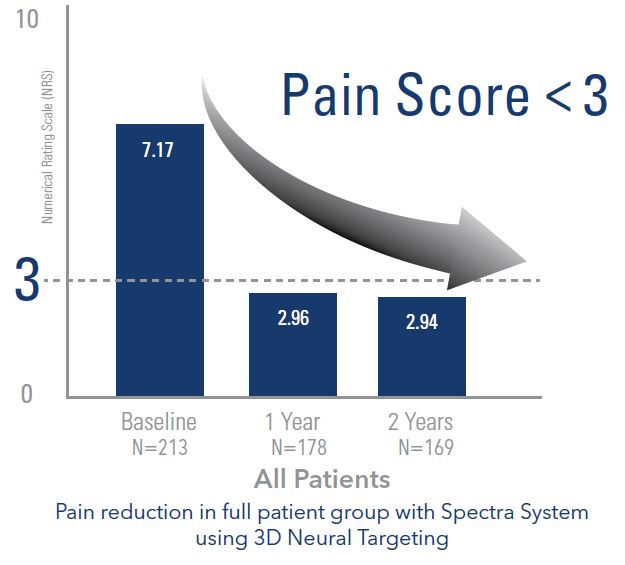
A 24-month analysis that compared the effectiveness of 3D neural targeting used in the Boston Scientific Precision Spectra™ System with an earlier generation SCS system also from Boston Scientific offers new insight on treating low back pain. Thirty to forty percent of the patients in the LUMINA Study had low back pain only, making the LUMINA Study one of the largest observational cohort (213 subjects) studies in SCS of patients with this type of pain.
The roundtable participants noted that new research offers hope for these patients and the potential to address the impact chronic pain has on their life. Low back pain is a prevalent condition which costs the United States more than $100 billion annually with two-thirds of that due to lost wages and decreased productivity.2,3
For patients with low back pain only, the use of 3D neural targeting resulted in approximately 70 percent better pain relief than the Boston Scientific previous generation system.4 Additionally, the LUMINA Study showed a significant decrease in average pain scores sustained over a two-year period.4
"Chronic pain conditions involving the low back are one of the most difficult types of pain to treat," Dr. North said. “The nerves that innervate the low back are very close to the nerves that innervate the rib. Older technologies were not able to precisely stimulate only those nerves. As the technology has evolved with the availability of neural targeting, I’m able to more precisely hone in on the source of my patient’s pain.”
The whole picture — how to measure pain accurately
Given the complex nature of pain, evaluating and measuring chronic pain is one of the key challenges physicians face. Many clinicians rely on the comparative pain scale to first assess a patient’s pain and then their response to treatment with SCS. While it helps physicians to understand how the patients are experiencing their pain, pain scores are subjective and fail to incorporate other factors that may influence how pain is impacting a patient’s life. The discussion noted the importance of considering both quality of life measures along with the relief they get with SCS.
“It amazes me how often my patient will begin with a pain intensity of 8 out of 10. Then they come back and it's 7 out of 10. I say, ‘well that's not very much.’ But their relief is 80 percent,” said Mark Wallace , M.D., chair of the division of Pain Medicine in the Department of Anesthesiology, University of California, San Diego. “That’s because pain intensity is a uni-dimensional measurement, whereas pain relief provides more qualitative factors that have a large impact on patients' quality of life, such as their mobility and quality of sleep."
“With opioids, you might get a reduction in the pain score, but you don’t get an improved health-related quality of life,” noted Simon Thomson, M.D., consultant in pain medicine and neuromodulation, Basildon and Thurrock University NHS Trust. “This is quite different from SCS, where the health-related quality of life and the pain score are maintained long term.”
With advancements in technology and new clinical information available, the SCS of today is a different treatment option than what existed as recently as five years ago. New data illustrates that SCS can effectively treat patients with low back pain, a common pain-related diagnosis. Clinicians also now recognize that pharmacologic agents may not be effective for certain types of pain such as neuropathic pain and many patients are actively seeking treatment options that do not involve opioids. As the impact of the opioid crisis on patients, families and communities continues to increase, the need to expand the treatment paradigm is growing. The roundtable discussion concluded with a consensus among physicians that it is time for the medical community to evaluate the patient pathway and reassess which patients are good candidates for SCS. They believe a collaborative approach across medical specialties combined with broader awareness of advancements in SCS treatment has the potential to deliver better long term relief to patients suffering from chronic pain.
- Institute of Medicine Report from the Committee on Advancing Pain Research, Care, and Education: Relieving Pain in America, A Blueprint for Transforming Prevention, Care, Education and Research. The National Academies Press, 2011. http://books.nap.edu/openbook.php?record_id=13172&page=1, http://www.nap.edu/read/13172/chapter/2. Accessed March 25, 2016.
- Katz Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am, 2006, 88(suppl 2):21-24.
- Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin, 2007, 25(2):353-371.
- Elias Veizi, MD, PhD, et al. “Spinal Cord Stimulation (SCS) with Anatomically Guided (3D) Neural Targeting Shows Superior Chronic Axial Low Back Pain Relief Compared to Traditional SCS—LUMINA Study.” Pain Medicine 2017; 0: 1-15.
US Indications for Use: The Boston Scientific Neuromodulation Spinal Cord Stimulator (SCS) Systems are indicated as an aid in the management of chronic intractable pain of the trunk and/or limbs, including unilateral or bilateral pain associated with the following: failed back surgery syndrome, intractable low back pain, and leg pain. Contraindications, warnings, precautions, side effects. The SCS Systems are contraindicated for patients who: are unable to operate the SCS System, have failed trial stimulation by failing to receive effective pain relief, are poor surgical risks, or are pregnant. Refer to the Instructions for Use provided with the SCS System or ControlYourPain.com for potential adverse effects, warnings, and precautions prior to using this product. Caution: Federal (U.S.) law restricts this device to sale by or on the order of a physician.
Outside of US Indications for Use: CAUTION: The law restricts these devices to sale by or on the order of a physician. Indications, contraindications, warnings and instructions for use can be found in the product labelling supplied with each device. Information for use only in countries with applicable health authority registrations. Material not intended for use in France.
Results from clinical studies are not predictive of results in other studies. Results in other studies may vary.
NM-428001-AA_APR2017
More articles on devices:
After Unveiling in MIT Lecture, Xenco Medical Founder Announces Launch of Virtual, Holographic System for Surgical Planning
Conmed EVP purchases 440 company shares — 5 insights
CyMedica Orthopedics enrolls 1st patient in clinical rehabilitation trial — 4 details